Let's talk aboutAre Homocysteine Levels Genetic?
What is homocysteine?
Homocysteine is an amino acid that plays a key role in important processes like making proteins. Vitamins B6, B12, and folate (also called B9) help convert homocysteine into other substances your body needs. When homocysteine levels get too high, it may indicate an increased risk of certain health conditions, such as cognitive decline and stroke.

What is the role of MTHFR mutations?
The MTHFR gene contains instructions for making an enzyme that’s important for how the body processes folate, which in turn helps recycle homocysteine into another amino acid called methionine. When the MTHFR enzyme is working properly, it helps convert folate into a form that helps break down homocysteine. However, some people have genetic variations in the MTHFR gene that can make this process less efficient, leading to slightly higher homocysteine levels.
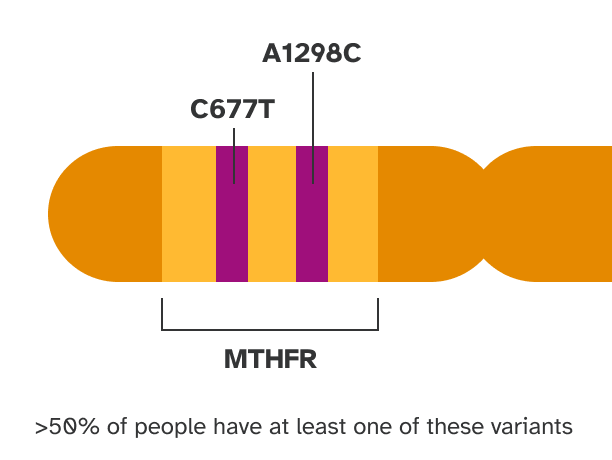
How can MTHFR variants impact homocysteine levels?
There are two common genetic variants in the MTHFR gene, called C677T and A1298C, that make the MTHFR enzyme less active. As a result, people with one copy of the C677T variant may have ~10% higher levels of homocysteine, and people with two copies may have ~30% higher levels, compared to people with no copies. These levels are still typically within the range considered normal or mildly elevated. The A1298C variant has not consistently been shown to impact homocysteine levels, but may have some impact when present along with a C677T variant.
MTHFR and misinformation
It’s important to know that misinformation about MTHFR is common. For example, claims that MTHFR variants are associated with a wide range of health risks are based on flawed research that has largely been disproven. The main health risk consistently associated with MTHFR variants is that people with two copies of the C677T variant have a slightly increased risk of having a pregnancy with neural tube defects such as spina bifida, although the overall risk is still very low.
In addition, little research exists to support claims that MTHFR variant carriers should take modified forms of folate such as 5-MTHF. MTHFR variant carriers can still process all forms of folate, and 5-MTHF has not been studied in clinical trials. Regardless of genetics, everyone who may become pregnant is recommended to take 400 micrograms of folic acid daily, which reduces the risk of neural tube defects. Learn more from the CDC.
Ways to take action
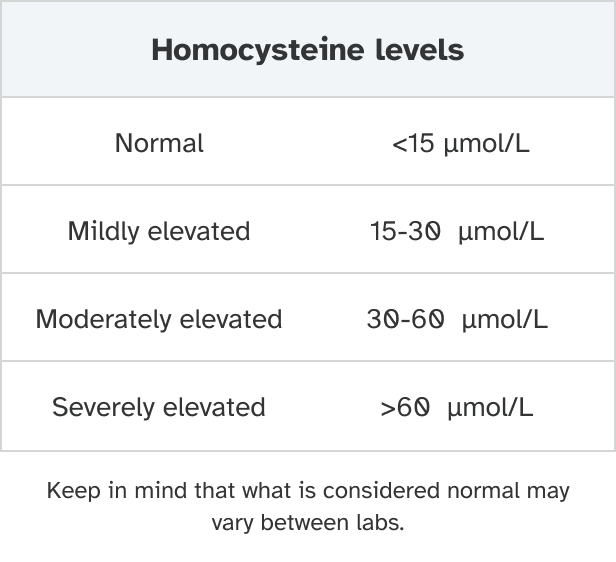
Most people with MTHFR variants are still expected to have homocysteine levels within the normal range. But for those who are concerned, a blood test can check homocysteine levels.
And it’s a good idea for everyone to get enough folate, which can help maintain healthy homocysteine levels. Most people can achieve this through a normal, varied diet that includes folate-rich foods like leafy green vegetables, eggs, legumes, and fortified breads and cereals. In addition, folic acid supplements (a form of folate) are recommended for all people who may become pregnant because they need higher daily amounts.
If you have high homocysteine or a folate deficiency, you may also benefit from a folic acid supplement to get the recommended daily amount of 400 micrograms of dietary folate equivalents (DFE). You can check your homocysteine levels at 23andMe.
Other factors that can impact your chances of developing high homocysteine
Besides genetics, several other factors can contribute to elevated homocysteine levels.
One important factor is vitamin deficiency — being deficient in vitamins B6, B12, or folate (also called B9) can increase the likelihood of having homocysteine levels that are too high. People who don’t regularly eat folate-rich foods like fortified grains and bread, legumes, and green leafy vegetables may be at increased risk of folate deficiency. And people who don’t eat animal products may be at increased risk of deficiency for vitamin B12. In addition, people with alcohol use disorder or digestive conditions like Crohn’s disease or celiac that impact nutrient absorption may be at increased risk of vitamin deficiencies.
Additional factors that can be associated with higher homocysteine levels include:
- Older age
- Smoking
- Heavy alcohol consumption
- Being male
- Certain health conditions, such as chronic kidney disease
In addition, a rare inherited condition called homocystinuria causes greatly increased levels of homocysteine. Homocystinuria is caused by different genetic variants than the common C677T and A1298C variants.
What do your genes say about your homocysteine levels?
The Homocysteine (MTHFR-Related) report* can help you learn what your genetics have to say about your likelihood of developing slightly elevated levels of homocysteine, as part of the 23andMe+ Premium Membership. 23andMe+ Premium includes everything in our Health + Ancestry Service plus new premium reports and features throughout the year.

23andMe+ Premium Membership Service
Learn more
Please note:
- The Homocysteine (MTHFR-Related) report does not diagnose elevated homocysteine or any health conditions and should not be used to make medical decisions.
- The report does not account for lifestyle or family history.
- The report does not account for every possible genetic variant that could affect your likelihood of developing elevated homocysteine.
References
Levin et al. (2016). “MTHFR: Addressing Genetic Counseling Dilemmas Using Evidence-Based Literature.” J Genet Couns. 25(5):901-11.
Martí-Carvajal et al. (2017). “Homocysteine-lowering interventions for preventing cardiovascular events.” Cochrane Database Syst Rev. 8(8):CD006612.
Moll et al. (2014). “Homocysteine and MTHFR Mutations.” Circulation. 132(1):e6-9.
Smith et al. (2018). “Homocysteine and Dementia: An International Consensus Statement.” J Alzheimers Dis. 62(2):561-570.