Is Depression Genetic?Explore Depression and what your DNA can tell you
What is depression?
Everyone can sometimes experience sadness, guilt, and other negative emotions in response to life’s ups and downs. But people with depression may experience negative emotions and other mental and physical symptoms that are intense, don’t go away over time, and make it hard to carry on the normal activities of daily life. The causes of depression are complex and not completely understood, but they are thought to include both biological differences in things like genetics, brain chemistry, and hormones, as well as life experiences and environmental stressors.
If you have been diagnosed with depression, know that you’re not alone. Depression is very common. About 1 in 5 people in the U.S. will be diagnosed with depression during their lifetime.
Find Out if Your Genetics Might Increase Your Likelihood for Developing Depression.

What are the symptoms of depression?
Depression symptoms can range from mild to severe, and may vary from person to person. Some common symptoms can include:
* Feeling sad, empty, hopeless, irritable, guilty, or other difficult emotions
* Loss of interest or pleasure in activities you used to enjoy
* Decreased energy
* Difficulty thinking or concentrating
* Difficulty sleeping or oversleeping
* Loss of or increase in appetite
* Aches and pains like headaches, backaches, or digestive symptoms that do not respond to treatment
* Thoughts of harming oneself, death, or suicide

Is depression genetic?
The likelihood of experiencing depression is impacted by many factors, both non-genetic and genetic. Some people may be more likely to experience depression than others, depending on their genetics. Depression can run in families, which means that a person has an increased chance of having depression if family members have the condition. A combination of many different genetic variants impact a person’s chances of experiencing depression. Individually, each of these variants only has a small impact on a person’s genetic likelihood, but that impact can grow when many variants are considered together. 23andMe takes into account more than 8,400 genetic markers to estimate the likelihood of having been diagnosed with depression.
For all individuals, genetic testing is available to identify variants linked to depression. Additional genetic factors may be discovered in the future.
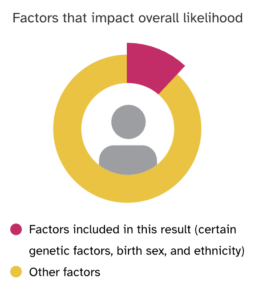
Depression is also impacted by many non-genetic factors. Genetics combine with other factors to influence an individual’s overall likelihood of developing depression. Examples of non-genetic factors can include:
- Many health conditions, including other mental health conditions
- Stressful life events
- Social isolation or lack of support
- Problems with alcohol, tobacco, or drug use
- Having a family history of depression or other mental health conditions
- Childhood adversity or maltreatment
- Experiencing discrimination due to race, sexual orientation, gender expression and identity, or other factors
- Gender: Cisgender women and transgender and non-binary individuals are more likely to be diagnosed with depression

What are some ways to manage depression?
While depression is impacted by some factors that can’t be changed—like genetics—it’s also impacted by some things that can, including lifestyle habits. Some healthy habits that can help people manage depression symptoms include:
- Seek social interaction and support from family, friends, and/or a counselor or other mental health professional. This is especially important during times of stress, such as major life changes or losses.
- Do your best to get active—exercise is very effective at improving mood.
- Practice good sleep habits, such as keeping your bedroom dark at night and getting sunlight during the day to strengthen your circadian rhythms.
- Explore stress-reduction and/or mindfulness techniques like meditation or yoga.
- Avoid using alcohol and tobacco, and if needed, consider getting help to quit.
- Engage in hobbies and other activities that are pleasurable, like getting a pet, listening to music, and spending time in nature, which have also been found to improve mood.
- Don’t face depression alone. Talk to a healthcare professional. Most cases of depression respond well to treatment with counseling, medication, or a combination of the two.
If you have any concerns or feel depressed, please reach out to a loved one or a healthcare professional like a primary care provider, clinical psychologist, mental health counselor, or genetic counselor.
If you’re in a crisis, call or text 988 in the U.S. or find a helpline in your area.
Here are some additional resources for you to find the help you or a friend or family member might need. Remember you are not alone, and there are people who can help you get the support you need. It’s OK to ask for assistance.
• 988 Suicide and Crisis Lifeline — formerly known as the National Suicide Prevention Lifeline, 988 provides free and confidential emotional support to people in suicidal crisis or emotional distress 24 hours a day, 7 days a week across the United States. The Lifeline is comprised of a national network of over 200 local crisis centers, combining custom local care and resources with national standards and best practices. They can provide support or connect you with local resources. Either call or text 988, or you can call 1-888-628-9454.
• Crisis Text Line — The Crisis Text Line is another free resource that’s available 24/7. If you’re not comfortable talking on the phone, you can text with a trained crisis counselor. To get started, text HOME to 741741.
• National Alliance on Mental Illness — The National Alliance on Mental Illness (NAMI) is an organisation that provides education, support, and advocacy. Their helpline is available Monday through Friday, 10am to 8pm ET, at 1-800-950-NAMI (6264). They also have a wealth of resources on their website, including information on depression and suicide.
• Therapy — Talking to a therapist can help if you’re struggling. An experienced therapist can help you navigate and find the best approaches to treating depression. Even if you don’t have insurance there are still options available, such as community mental health centers or sliding-scale therapy.
Remember, it’s okay to reach out for help. You don’t have to go through this alone. There are people who care about you and want to help you get through this.
Find out if your genetics might increase your likelihood of developing Depression
Curious whether you have an increased likelihood of experiencing depression based on your genetics? Find out more with the Depression report (Powered by 23andMe Research), part of the 23andMe+ Premium membership. 23andMe+ Premium includes our Health + Ancestry Service plus new premium reports and features throughout the year.

23andMe+ Premium
Please note:
- This report does not diagnose depression and should not be used to make medical decisions.
- The report was developed by 23andMe scientists using data and insights gathered from thousands of customers who consent to participate in our research. Reports based on 23andMe research provide an estimate of your likelihood of having been diagnosed with a condition based on your genetics and other factors. This report does not account for life experiences or family history.
- The report does not account for every possible genetic variant that could affect your likelihood of being diagnosed with depression.
References:
- American Psychiatric Association. “What is depression?” Retrieved March 8, 2023, from https://www.psychiatry.org/patients-families/depression/what-is-depression.
- American Psychological Association. “Depression.” Retrieved March 8, 2023, from https://www.apa.org/topics/depression.
- Centers for Disease Control and Prevention. “Managing Depression.” Retrieved March 17, 2023, from https://www.cdc.gov/learnmorefeelbetter/programs/depression.htm.
- Cuijpers P et al. (2019). “Psychological Treatment of Depression in Primary Care: Recent Developments.” Curr Psychiatry Rep. 21(12):129.
- Hasin DS et al. (2018). “Epidemiology of Adult DSM-5 Major Depressive Disorder and Its Specifiers in the United States.” JAMA Psychiatry. 75(4):336-346.
- Kvam S et al. (2016). “Exercise as a treatment for depression: A meta-analysis.” J Affect Disord. 202:67-86.
- Luca A et al. (2013). “Sleep disorders and depression: brief review of the literature, case report, and nonpharmacologic interventions for depression.” Clin Interv Aging. 2013;8:1033-9.
- Mayo Clinic. “Depression (major depressive disorder).” Retrieved March 8, 2023, from https://www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007.
- National Alliance on Mental Illness. “Depression.” Retrieved March 8, 2023, from https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Depression.
- National Institute of Mental Health. “Depression”. Retrieved March 8, 2023, from https://www.nimh.nih.gov/health/topics/depression.
- Sarris 2014. “Lifestyle medicine for depression.” BMC Psychiatry. 2014 Apr 10;14:107.
- Schuch FB et al. (2016). “Exercise as a treatment for depression: A meta-analysis adjusting for publication bias.” J Psychiatr Res. 77:42-51.
- Substance Abuse and Mental Health Services Administration. “SAMHSA’s National Helpline.” Retrieved March 17, 2023, from https://www.samhsa.gov/find-help/national-helpline.